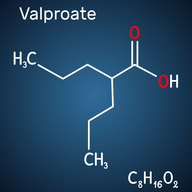
A Concentrated Form of Valproate to be Delivered via Bone for the Treatment of Hemorrhagic Shock
TECHNOLOGY NUMBER: 2019-471
OVERVIEW
Higher doses of valproic acid (VPA) improve survival in traumatic brain injury (TBI)- Both higher total doses as well as higher dose rates favorably affect outcomes in a swine model
- The investigators increased dosing while avoiding deleterious cardiac effects of VPA
BACKGROUND
Injuries are the leading cause of death for young people in the United States, and traumatic brain injury (TBI) results in 2.8 million emergency department visits per year. In current military conflicts, TBI is also a significant cause of morbidity and mortality. Unfortunately, current treatments for TBI are mostly supportive in nature, without any specific therapy that can improve survival or attenuate the extent of brain damage. Valproic acid (VPA), long used as an anti-epilepsy medication, has been shown to improve survival following lethal hemorrhage, polytrauma, septic shock, ischemia-reperfusion (I/R), and TBI. VPA is a histone deacetylase inhibitor, and the mechanism of action by which it improves survival is thought to result from its ability to cause acetylation of nuclear and cytoplasmic proteins. The current FDA approved dose is 20-60 mg/kg, while the current regulatory label suggests intravenous infusion at concentrations <100 mg/mL at a minimum infusion duration of 60-minutes. Delivery of higher doses raise concerns about drug toxicity and adverse effects. Still, existing data regarding the potential benefits to a more accelerated dose delivery suggests the need for additional research into this approach.
INNOVATION
Researchers have discovered that high dose valproic acid (VPA) shows survival benefits when delivered via intravenous infusion in a swine model of lethal hemorrhage, polytrauma, and traumatic brain injury (TBI). Previous studies using intravenous dosing of VPA at a rate of about 140 mg/kg to healthy human volunteers shows tolerability. This dose of VPA can improve neurocognitive outcomes following TBI that decreases hemorrhagic shock, neural apoptosis, and brain inflammation while promoting neural plasticity. The current investigation reveals that survival was improved with higher total doses and an increased dose rate delivery of VPA. The investigators suggest an ability to overcome the potentially deleterious cardiovascular effects of VPA by creating a drug-delivery autoinfusion device that contains a concentrated and therefore lower volume version of valproate, that is self-contained, and which permits a controlled rate of delivery. VPA is also known to improve survival in lethal models of sepsis by helping to attenuate end organ injury caused by shock. In summary, the described approach reveals the survival benefit of a single dose of VPA given early after injury as demonstrated in a model of hemorrhage and polytrauma.