Esophageal Luminal Monitoring and Retraction System
TECHNOLOGY NUMBER: 2020-167
OVERVIEW
Use of luminal esophageal retraction probe that monitors temperature- Provides the ability to move the esophagus away from the atrial wall
- Measures and decreases esophageal toxicity due to cardiac ablation
BACKGROUND
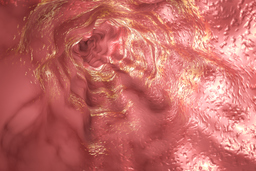
The use of endoscopic ultrasound with transesophageal catheter ablation has emerged as a common and effective strategy for managing symptomatic atrial fibrillation (AF) which is refractory to drug therapy. The procedure does not normally cause toxicity, though thermal injury to the esophagus may occur, especially when performing ablation for lesions located on the posterior wall of the left atrium. These instances of esophageal injury can range in severity from mild erythema to ulcer formation, with the rare potential to progress into an atrial esophageal fistula.
Though the rate of esophageal fistula is less than 0.5% of patients following this procedure, sequelae can include significant morbidity or death. Also, thermal-mediated damage to the vagal plexus can result in gastric dysmotility and gastroparesis. Several existing techniques can be utilized to minimize damage to the esophagus, including luminal esophageal temperature (LET) monitoring, the use of a lower power or duration ablation, irrigating the esophagus with cold water, or mechanical esophageal deviation. Given limitations to each of these approaches, a need exists to improve the protection of the esophagus during cardiac ablation procedures.
INNOVATION
Researchers at the University of Michigan have created a luminal esophageal retraction probe that can monitor tissue properties including temperature and move the esophagus away from the atrial wall. The invention provides the ability to visualize three-dimensional changes of the esophageal wall, it measures underlying tissue properties caused by thermal effects to detect tissue damage, and it documents esophageal wall deformation caused by mechanical pressures created by the ablation catheter while inside the heart. These capabilities will allow physicians to better determine the location of the ablation catheter in relation to the esophageal wall and will also provide improved early detection of thermal damage while quantifying thermal damage.